You fall asleep just fine.
But then, suddenly — 3 AM.
Your eyes open.
Your mind feels alert.
Your heart may be racing slightly.
And falling back asleep feels impossible.
This pattern is extremely common during perimenopause — and it’s not random insomnia.
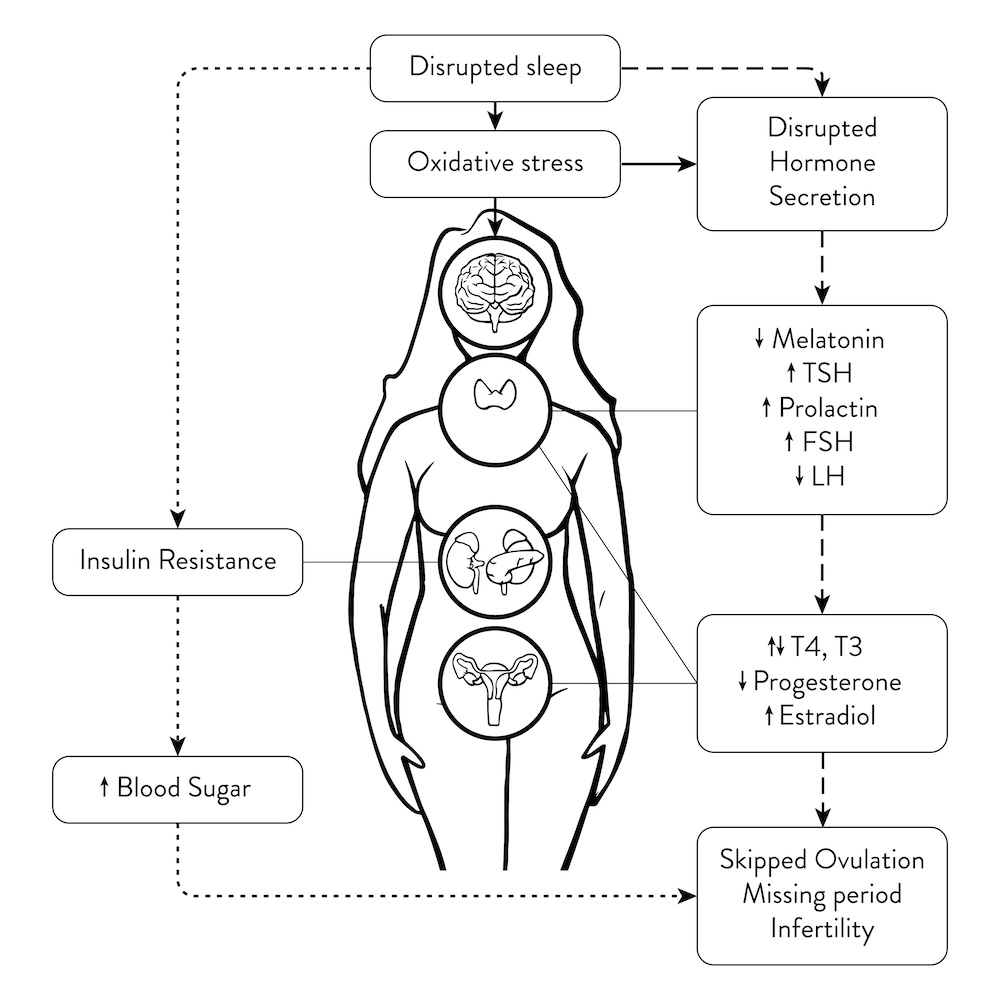
Waking up at 3 AM is one of the most specific metabolic and hormonal signals of perimenopause, driven by changes in blood sugar, cortisol, estrogen, and progesterone.
The Science Behind the 3 AM Wake-Up
In a healthy rhythm, cortisol stays low overnight and slowly rises toward morning.
During perimenopause, this rhythm often breaks.
1. The Blood Sugar Crash (Main Trigger)
Around 2–4 AM, liver glycogen (stored glucose) can drop too low.
When the brain senses low fuel, the body responds by releasing:
- Cortisol
- Adrenaline
This forces glucose into the bloodstream — but it also jolts you awake.
This is why 3 AM wake-ups often feel sudden and alert, not groggy.
📎 Read More: Insulin Resistance Belly vs Cortisol vs Thyroid Belly
📎 Read More: Healthy Foods That Spike Blood Sugar
2. Progesterone Decline (Loss of Natural Sedation)
Progesterone supports GABA — the brain’s calming neurotransmitter.
During perimenopause:
- Progesterone is often the first hormone to drop
- Sleep becomes lighter
- The body wakes more easily to stress signals
Without progesterone’s calming effect, cortisol spikes are harder to tolerate.
📎 Read More: Why Perimenopause Feels Like a Second Puberty
3. The Histamine Factor
Histamine naturally rises in the early-morning hours.
Lower estrogen makes the body more sensitive to histamine.
This can trigger:
- Wakefulness
- Racing thoughts
- Itching
- Heat sensations
📎 Read More: The Estrogen–Histamine Loop
📎 Read More: Itchy Ears During Perimenopause: Causes & Simple Relief

Falling Asleep vs Waking at 3 AM (Important Difference)
| Sleep Pattern | Likely Cause |
|---|---|
| Trouble falling asleep | High evening cortisol |
| Waking at 2–4 AM | Blood sugar + cortisol spike |
| Waking hot or sweaty | Estrogen fluctuation |
| Light, restless sleep | Progesterone decline |
If you fall asleep easily but wake up alert, the issue is metabolic — not mental.
How to Stop the 3 AM Wake-Up
Generic sleep hygiene alone doesn’t fix this.
You must stabilize the underlying physiology.
1. The Bedtime “Safety Snack” (Immediate Fix)
A small protein-focused snack before bed can prevent overnight glucose drops.
Good options:
- Nut butter
- Plain Greek yogurt
- A small protein portion
Avoid:
- Sugary snacks
- Alcohol
- Late desserts
2. Morning Light Exposure (Circadian Reset)
Seeing natural light soon after waking helps anchor cortisol to the morning, not the night.
This improves melatonin release later that evening.
📎 Read More: Cortisol & Morning Coffee Timing
3. Cool the Sleep Environment
Body temperature must drop to maintain deep sleep.
Helpful strategies:
- Cooler bedroom
- Breathable bedding
- Warm shower before bed (followed by cooling)
If You Wake Up Anyway (Damage Control)
If you wake at 3 AM:
- Do not check your phone
- Avoid bright light
Helpful options:
- Slow nasal breathing
- Gentle body-based relaxation
- Lying still with eyes closed (non-sleep deep rest)
These calm the nervous system and may allow sleep to return.

When to Seek Medical Support
Consult a clinician if:
- Insomnia persists for months
- You snore loudly or gasp at night
- You experience leg discomfort or severe anxiety
Hormonal insomnia is common — but other conditions can coexist.
📎 Read More: Sleep Apnea & Belly Fat
Related Reading
📎 Read More: Itchy Ears During Perimenopause: Causes & Simple Relief
📎 Read More: The Estrogen–Histamine Loop
📎 Read More: Cortisol Crash in the Afternoon
📎 Read More: Wearable Metrics That Reveal Hormone Imbalance
Health Disclaimer
This article is for general wellness education only.
Persistent insomnia should be evaluated by a licensed healthcare professional.