Everyone talks about hot flashes.
So when you suddenly feel bone-deep cold, shivering in a warm room, it can be confusing — even alarming.
If you’re in your late 30s or 40s, these episodes are often cold flashes linked to perimenopause, not “random chills” and not anxiety.
🔎 Key Takeaways (TL;DR)
- Cold flashes in perimenopause are commonly driven by estrogen drops and cortisol spikes
- They feel different from hot flashes and often happen at night or during stress
- Stabilizing blood sugar, sleep timing, and the nervous system can reduce episodes
Why Cold Flashes Happen in Perimenopause (The Body-First Explanation)
Cold flashes don’t start in the mind.
They start in the temperature-regulation system.
During perimenopause:
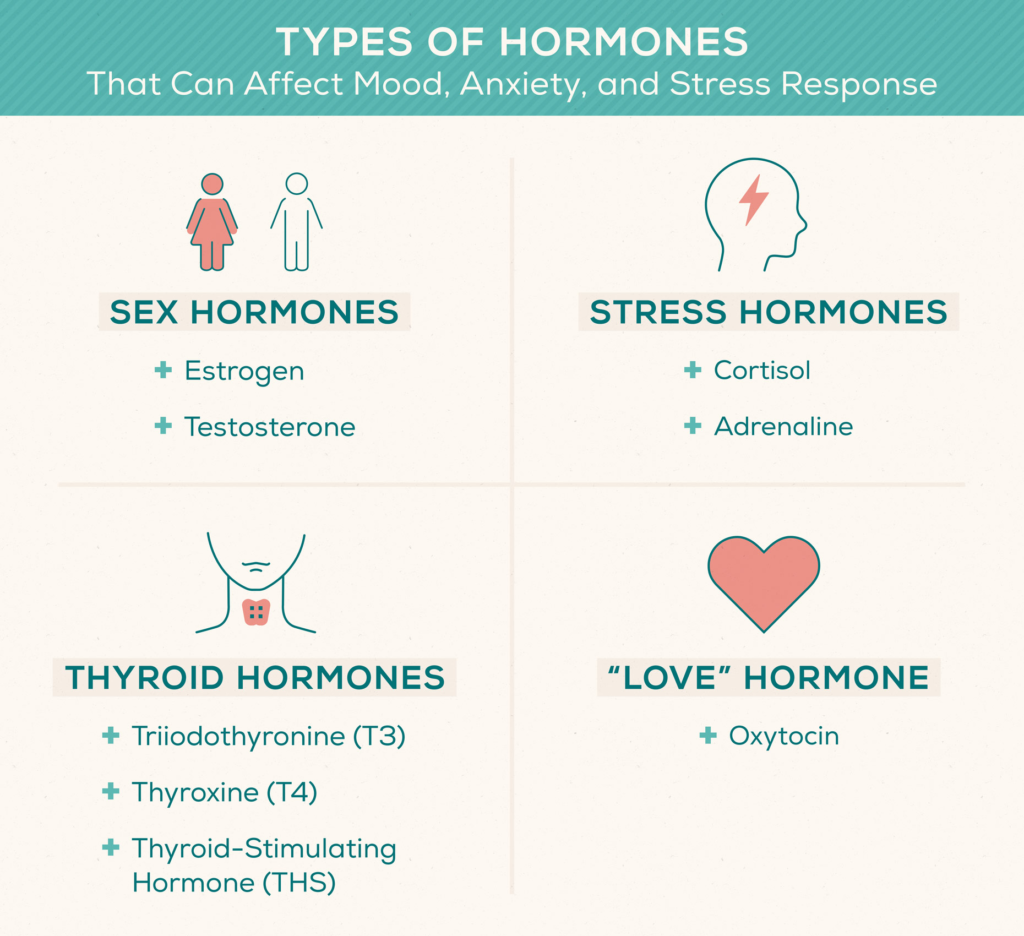
- Estrogen fluctuates unpredictably
- Cortisol becomes more reactive
- Blood vessel control becomes unstable
Estrogen normally helps regulate vasodilation (how blood flows to skin).
When estrogen dips suddenly, blood vessels may constrict instead of relax, causing a rapid sensation of cold.
At the same time, cortisol surges can pull blood away from the skin — intensifying chills.
📎 Read More: Why Perimenopause Feels Like a Second Puberty
Cold Flashes vs Hot Flashes: What’s the Difference?
| Feature | Cold Flashes | Hot Flashes |
|---|---|---|
| Sensation | Sudden chills, shivering | Heat, sweating |
| Blood Flow | Constriction | Sudden dilation |
| Timing | Night, stress, fatigue | Day or night |
| Trigger | Estrogen drop + cortisol | Estrogen fluctuation |
Cold flashes are not the opposite of hot flashes — they’re a different stress-hormone response.
Why Cold Flashes Often Hit at Night
Many women notice chills:
- When lying down
- After waking suddenly
- Around 2–4 AM
At night:
- Blood sugar may dip
- Cortisol rises to compensate
- Adrenaline activates temperature control
This combination can trigger intense cold waves, even without fever.
📎 Read More: Wired But Tired at Night: Why Your Cortisol Is Spiking
📎 Read More: Perimenopause Insomnia: Why You Wake Up at 3 AM

Is This Normal? (Yes — and Here’s How It Feels)
Yes. Cold flashes are commonly described as:
- Icy waves moving through arms or legs
- Bone-deep cold, not surface chill
- Shivering without fever
- Needing blankets even in warm rooms
This doesn’t mean infection, anxiety disorder, or “something serious.”
It reflects hormonal stress response changes.
The Blood Sugar–Cortisol–Cold Flash Loop
Low blood sugar can worsen chills.
When glucose drops:
- The brain senses danger
- Cortisol rises
- Blood is redirected away from skin
This makes cold sensations feel stronger and longer.
Helpful steps include:
- Protein with dinner
- Avoiding late-night sugar or alcohol
- Consistent meal timing
📎 Read More: Hormonal Belly Fat (Estrogen vs Cortisol)
What Helps Reduce Cold Flashes Naturally
You can’t force warmth — but you can restore regulation.
Helpful strategies:
- Gentle breathing with long exhales
- Light movement (not intense cardio)
- Stable sleep and wake times
- Warm protein-rich evening meals
The goal is nervous system safety, not stimulation.
📎 Read More: Stress Weight Gain (Even With Clean Eating)
FAQs
Can anxiety cause cold flashes?
Anxiety can amplify them, but hormonal stress response changes are usually the root.
Do cold flashes mean menopause is ending?
No. They often appear during fluctuating hormone phases, not just late stages.
Should I worry about infection?
If chills occur with fever or illness, consult a doctor. Hormonal cold flashes happen without fever.

Related Reading
📎 Read More: Why Perimenopause Feels Like a Second Puberty
📎 Read More: Wired But Tired at Night: Why Your Cortisol Is Spiking
📎 Read More: Perimenopause Insomnia: Why You Wake Up at 3 AM
📎 Read More: Hormonal Belly Fat (Estrogen vs Cortisol)
Health Disclaimer
This article is for educational purposes only and does not constitute medical advice.
Cold flashes can overlap with other conditions. Consult a qualified healthcare professional for diagnosis or treatment.