Out of nowhere, your heart starts racing.
Your chest feels tight.
Your body feels flooded with fear — without a clear reason.
If you’re in your late 30s or 40s, these episodes may not be “random anxiety.”
They often reflect how perimenopause rewires the stress response.
Many women experience panic attacks for the first time during this phase — even without a prior anxiety history.
Why Panic Attacks Feel Different in Perimenopause
Hormonal panic doesn’t always start in the mind.
It often starts in the body first.
During perimenopause:
- Estrogen and progesterone fluctuate unpredictably
- Cortisol becomes more reactive
- The nervous system shifts toward “threat mode”
This creates sudden physical panic sensations that don’t match your thoughts.
📎 Read More: Why Perimenopause Feels Like a Second Puberty
The Hormonal Stress Response Explained
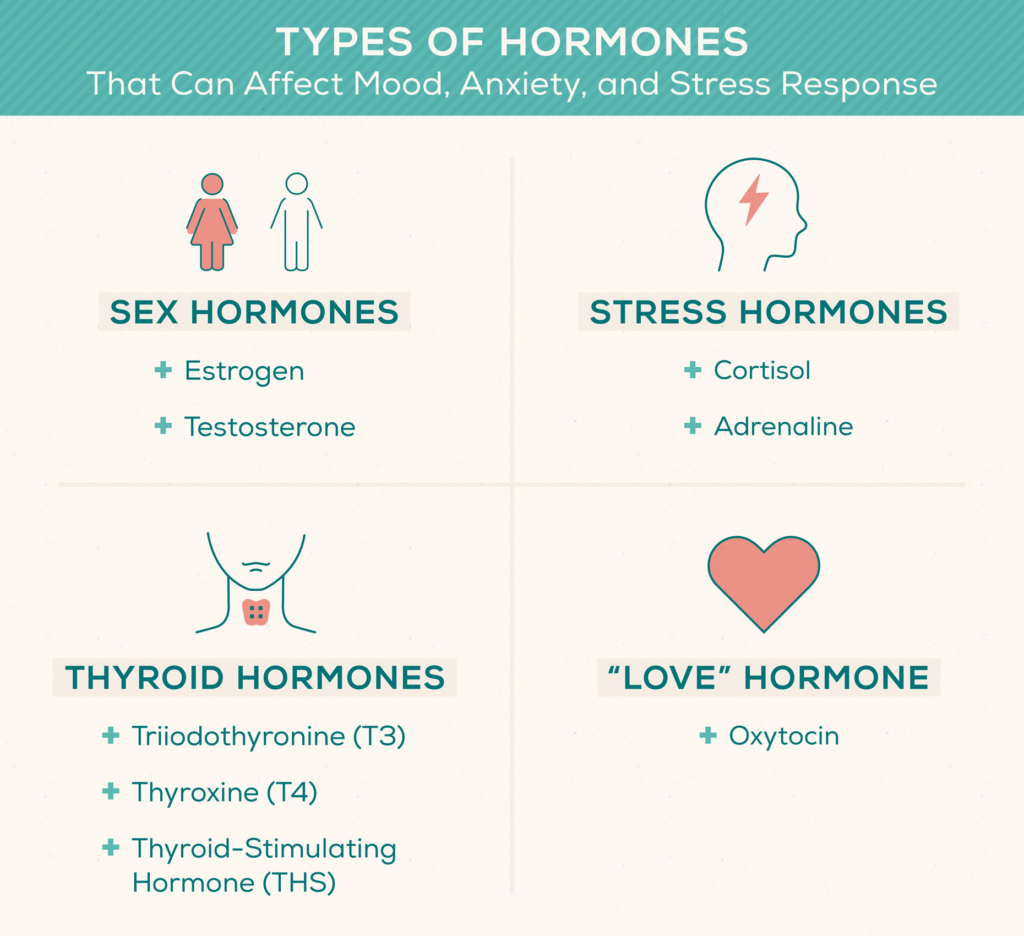
Your stress response relies on balance between:
- Cortisol (alertness)
- Progesterone (calming)
- Estrogen (stress buffering)
As progesterone drops first:
- GABA calming signals weaken
- Cortisol effects feel stronger
- Adrenaline surges more easily
The result can feel like a panic attack without a trigger.
📎 Read More: Cortisol Symptoms
How Hormonal Panic Differs From Classic Anxiety
| Feature | Hormonal Panic | Typical Anxiety |
|---|---|---|
| Onset | Sudden, physical | Thought-driven |
| Trigger | Often none | Worry or fear |
| Timing | Night / early morning | Anytime |
| Relief | Body regulation helps | Cognitive tools help |
If panic feels physical-first, hormones are often involved.
📎 Read More: Wired But Tired at Night: Why Your Cortisol Is Spiking
Why Panic Often Hits at Night or Early Morning
Hormonal panic frequently aligns with cortisol timing issues.
At night:
- Blood sugar can dip
- Cortisol surges to compensate
- Adrenaline spikes wake the nervous system
This can cause:
- Panic on waking
- Racing heart at 2–4 AM
- A sense of impending doom
📎 Read More: Perimenopause Insomnia: Why You Wake Up at 3 AM
📎 Read More: Cortisol Crash in the Afternoon

The Blood Sugar–Cortisol–Panic Loop
Low blood sugar is a common but missed trigger.
Many women discover their “panic attack” is actually a blood-sugar drop. Using an OTC CGM (like Dexcom Stelo) can help spot these dips before symptoms escalate.
When glucose drops:
- The brain senses danger
- Cortisol and adrenaline rise
- Panic sensations follow
This is why panic may improve with:
- Balanced meals
- Protein at dinner
- Avoiding late sugar or alcohol
📎 Read More: Stress Weight Gain (Even with Clean Eating)
Weird Physical Sensations That Precede Hormonal Panic
For many women, panic doesn’t begin as a thought — it begins as a strange physical sensation that feels alarming and unfamiliar. These symptoms are common in perimenopause and are low-competition, high-intent searches in the US.
Internal Vibrations or Buzzing Sensation
You may feel an internal “buzz,” humming, or vibration — especially when lying still at night.
This often reflects nervous system hyper-excitability as estrogen and progesterone fluctuate, lowering the brain’s calming (GABA) signals.
Common search terms: “vibrating feeling perimenopause”, “internal buzzing anxiety”
Electric Shocks or “Zaps”
Sudden jolt-like sensations in the chest, head, or limbs can occur right before a panic wave.
These “zaps” are linked to rapid adrenaline surges and altered nerve signaling during hormonal transitions.
Common search terms: “perimenopause electric shocks”, “anxiety zaps hormones”
Crawling Skin (Formication)
A sensation like insects crawling on or under the skin can feel terrifying if you’ve never experienced it.
Hormonal shifts can increase histamine release and nerve sensitivity, amplifying this sensation during stress.
Common search terms: “formication perimenopause”, “crawling skin anxiety hormones”
Phantom Smells (Phantosmia)
Smelling smoke, chemicals, or something “off” when nothing is there can precede anxiety or panic.
Estrogen affects the olfactory system and limbic brain, which explains why this can appear during perimenopause.
Common search terms: “phantom smells perimenopause”, “phantosmia anxiety hormones”
Important: These sensations are real, physical, and hormone-linked — not imagined. Recognizing them early can prevent a full panic cascade.
📎 Read More: Cortisol Symptoms
📎 Read More: Wired But Tired at Night: Why Your Cortisol Is Spiking
What Helps Calm Hormonal Panic (Body-First Approach)
You can’t “think” your way out of hormonal panic.
You need to signal safety to the nervous system.
Helpful strategies:
- Slow, extended exhale breathing
- Gentle movement (not intense exercise)
- Consistent sleep timing
- Stable blood sugar
These approaches calm the body first — then the mind follows.

Why This Doesn’t Mean You’re “Anxious”
Many women fear these symptoms mean:
- Anxiety disorder
- Loss of control
- Mental health decline
But hormonal panic reflects biology, not personality.
As hormones stabilize, panic often reduces or resolves with proper support.
📎 Read More: Insulin Resistance Belly vs Cortisol Belly vs Thyroid Belly: The Body Shape Map
When to Seek Professional Support
Get medical support if:
- Panic is frequent or worsening
- Symptoms include fainting or chest pain
- Sleep is severely disrupted
Rule out other conditions — but don’t dismiss the hormonal connection.
Related Reading
📎 Read More: Why Perimenopause Feels Like a Second Puberty
📎 Read More: Wired But Tired at Night: Why Your Cortisol Is Spiking
📎 Read More: Perimenopause Insomnia: Why You Wake Up at 3 AM
📎 Read More: Cortisol Symptoms
Health Disclaimer
This article is for general wellness education only.
Panic symptoms can overlap with other conditions. Consult a licensed healthcare professional for diagnosis or treatment.